The Expense of Charting:
How Much Time and Money Does Charting
Actually Cost Your Medical Practice?

We are all familiar with the saying that “the job’s not done until the paperwork is through.” Nowhere does this feel more applicable than in the medical industry. Doctors and medical practitioners are faced with an avalanche of paperwork each and every day. Precious time is required for prescriptions, correspondence, routine office paperwork, employee evaluations, and administrative functions. In 2016, Health Affairs presented the results of a study which found that the time physician practices spend tracking and reporting quality measures to Medicare and private health insurers amounted to over $15 billion per year.
And that does not even take into consideration the number one job of medical care – charting. Accurate and prompt charting is required to register patient complaints, memorialize practitioner impressions from the patient visit, assess lab work and test results, and develop an effective treatment plan. The hope is that better charting leads to improved care, but it is also helpful in dealing with other providers and insurance companies. On the practical side, charts can help meet many of the updated government reporting requirements and provide back-up documentation in the case of any legal claims.
The problem is that creating a perfect chart that can meet all these needs takes a lot of time and effort. Hours must be carved out of the daily schedule to address this need – hours that are taken from revenue-producing activities and redirected to charting. Practices that still rely on paper charts, or those that use a dictation/transcription process for their charting, face other negatives:
- There is a heavy cost involved in maintaining paper charts: Someone has to pull the chart for the appointment, notes have to be added in some way, and the chart has to be filed again. Referrals may require additional time for copying and forwarding printed materials, and personnel must manually add test results. There is a high cost for paper contents, and the sheer size of charts requires a lot of office space for storage. Charts must be maintained for a specific period of time, so the required space grows as the practice grows.
- They are inefficient: The practitioner has to look through the entire chart prior to an appointment. Separate notes have to be written for every test or lab test ordered. Incomplete charts may mean that others in the practice do not see the entire picture, or they might order tests and prescriptions that are not in accord with the
stated treatment plan. - They can get lost: A chart might be temporarily “misplaced,” but it can mean a crucial delay in treatment if the chart is not found within a reasonable period of time.
- Provider notes are not accessible to patients and other practitioners: Government regulations require a move toward interoperability and an increase in sharing information with patients.
It is also hard to track follow-up care or manage complex cases with poor charting techniques. At the very worst, a symptom can be missed that leads to a misdiagnosis and a lapse in care. In response to these concerns, more practices now turn to the efficiencies of Electronic Health Records (EHRs), but care must be taken in selecting a provider as a poor EHR system can cause as many problems as paper charts.
The Cost of an Inefficient EHR System
With the changes in how much information is required when documenting patient encounters, practitioners constantly have to balance actual patient care with tedious documentation of that patient care. According to thehappymd.com’s RAND Study, “the majority of physicians who interacted with EHRs directly described cumbersome, time-consuming data entry” as one of the 9 Reasons Physicians Hate EMR. Complaints of investing 15-20 minutes to complete a visit note are not uncommon, and this creates disruptions to not only office services and productivity, but also to the physician’s private life, as well as their mental health and well-being.
What effect does this have on the practice’s profitability, and what does it mean for a provider’s personal life? Let’s use an example of a practice seeing 20 patients a day in 15 minute increments. Now let’s factor in that each one of those visits requires 15 minutes to complete the encounter note in an EMR:
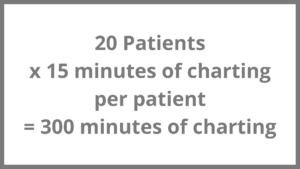
If that sounds like a lot, it is. That means the provider is spending five hours a day documenting visits instead of practicing medicine, training employees, reading medical journals, or just enjoying life. This time investment means that the provider is not performing billable services – even though the practice is still operating at full gear, with money going out the door every minute.
Time and Money Savings with an Efficient EHR System
The nice thing about technology is that even though the conversion to EMR and meeting CMS requirements have definitely made it slower to chart, practitioners also have access to tools that can actually save time and money. Whatever time is saved can also be converted to seeing more patients and making the practice more profitable, or even getting back personal time to spend with family and friends.
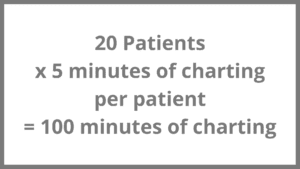
By using a more text-based EMR such as Amazing Charts, and charting using dictation software like Dragon, practitioners can significantly decrease the time it takes to complete encounter notes, all while still meeting the guidelines and requirements needed to maximize billing. A two-problem full encounter visit using one of these systems can now easily be completed in 3-5 minutes. Now let’s run the model shown above with a five minute encounter completion time:
Improved Charting Practices Can Lead to Better Patient Care and Improved Practice Profitability
Three additional hours per day is a substantial figure. If just one of those hours is used to see four more patients, at an estimated $100 per visit, that results in an additional $400 per day of practice revenue. Continuing the math, the practice could experience an additional $2000 per week, and $104,000 per year. By spending too much time charting, practices are actually losing over $100,000 per year.
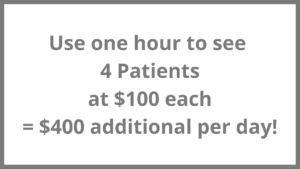
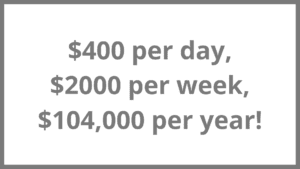
Three additional hours per day is a substantial figure. If just one of those hours is used to see four more patients, at an estimated $100 per visit, that results in an additional $400 per day of practice revenue. Continuing the math, the practice could experience an additional $2000 per week, and $104,000 per year. By spending too much time charting, practices are actually losing over $100,000 per year.

The results are quite astonishing. If a practitioner is charting at a rate of 15-20 minutes per encounter, and that figure is cut by 10 minutes each, the practice in essence would realize a $100,000 increase in revenue while the practitioner would actually be working over 500 hours less. That leads to the happy conclusion of making more money, and also having more time available to invest in other activities.
The Components of an Efficient EHR System
An efficient EHR system should enable clinicians to chart in the fastest way possible and with the least number of clicks, while also keeping the cost affordable for small practices.
Charting
The clinician should be able to quickly get to critical patient information with fewer clicks. The system should provide easy, one-click access to chart summaries, lab results, referral summaries, and past encounter summaries so there is no need to redocument the same information at every interaction.
Templates
Templates enable the user to work quickly and easily, and minimize the risk that the notes all end up being essentially the same. They are put in place to eliminate the need to click through finding after finding, or navigating through menu after menu.
e-Prescribing
The charting solution should contain a robust and built-in e-Prescribing module to make it easier for the provider to get needed medications to the patient more quickly.
Scheduling
An intuitive scheduler can be integrated into the EHR system to book, reschedule, and document missed and no-show appointments. This allows the provider to set appointment types and duration and quickly rebook appointments by jumping ahead four weeks, six weeks, one year, etc. This capability is particularly important in the case of chronic care management patients.
Patient Portal
In accordance with increased communication requirements an enhanced EHR system allows the provider to work with patients electronically to exchange messages, share visit summaries, test results and educational materials. This increases interaction levels with patients before and after office visits, and decreases the amount of time staff spends booking appointments and making copies of patient medical records.
Messaging
Intra-office messaging is a critical component of an EHR. Charts should be accessible and editable within any inbox to any users with appropriate access.
Reporting
The physician should have the capability to use the EHR system to query the database and find all patients meeting certain criteria.
Billing
The EHR can be used to automatically create and store an electronic superbill for billing purposes.
Most physicians didn’t go to medical school so they could complete more paperwork – they went to school so they would be able to help people feel better. They should not be kept from this pursuit because they are spending too much time completing thousands of documents and inefficiently completing patient charts.
Increased charting effectiveness not only leads to better patient care, it also means that the practice can increase revenue, avoid CMS penalties, achieve interoperability, close health care gaps, and increase patient engagement. All that, and even a little extra time left over – just by paying more attention to the type of EHR system in use.

